Pulmonary Fibrosis has no Cure: Could a Cancer Drug Hold the Answer?
Researchers at Tulane University have identified a potential new way to treat idiopathic pulmonary fibrosis (IPF), a deadly and currently incurable lung disease that affects more than 3 million people worldwide.
IPF is rapidly progressive and causes scarring in the lungs, making it difficult to breathe. Approximately 50% of patients die within three years of diagnosis, and current treatments can only slow the disease – not stop or reverse it.
In a study published in the Journal of Clinical Investigation, Tulane scientists found that an FDA-approved cancer drug may help the immune system clear out the damaged cells that cause the lung scarring, potentially restoring lung function in patients with the disease.
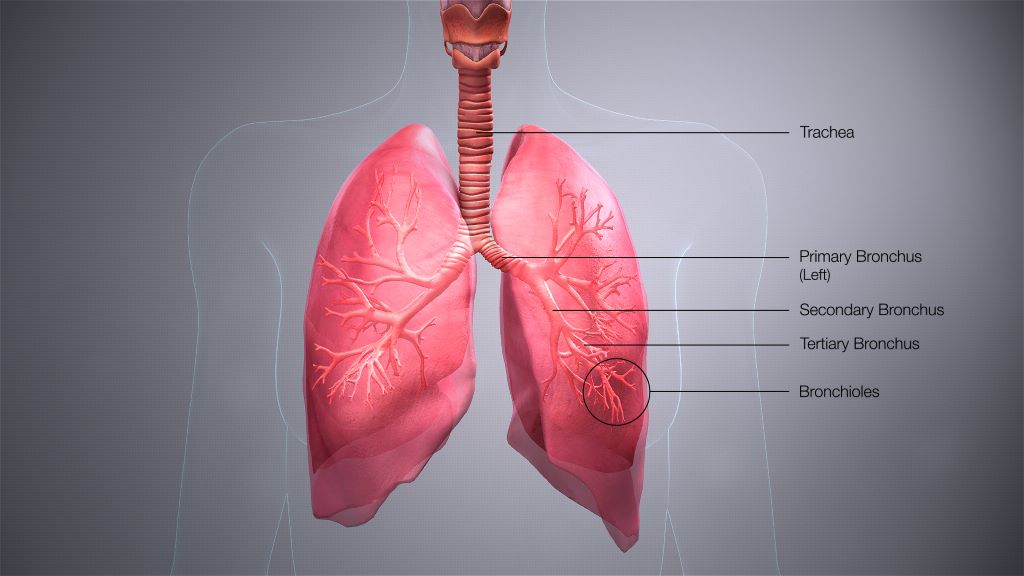
In healthy lungs, specialised cells called fibroblasts help repair lung tissue. But in people with IPF, some fibroblasts and nearby epithelial cells stop functioning properly. These so-called “senescent” cells no longer divide or die as they should. Instead, they build up and contribute to stiff, scarred lungs.
Tulane researchers discovered that these senescent cells appear to accumulate when the immune system’s natural ability to remove them is blocked. The culprit: a protein called CTLA4, which acts as an emergency brake on immune system activity.
By using ipilimumab — an immunotherapy drug currently used to treat various cancers — the researchers were able to block CTLA4 in mice. This released the “brakes” on certain immune cells called T cells, reactivating their ability to clear out the senescent fibroblasts. As a result, the mice showed significantly improved lung tissue regeneration and reduced scarring.
“The CTLA4 protein normally functions to prevent excessive inflammation by blocking overactive T cells,” said senior author Dr. Victor Thannickal, professor and Harry B. Greenberg Chair of Medicine at Tulane University’s John W. Deming Department of Medicine. “Too much of this ‘blocker protein’ may result in losing the ‘good’ inflammation that is needed to remove senescent cells. What we’re doing is blocking the blocker.”
The researchers zeroed in on CTLA4 as a potential therapeutic target when they analyzed both human and mouse IPF lung tissue and found unusually high levels of CTLA4 on the T cells in the areas where scarring was most prevalent.
Mice that received ipilimumab showed significantly improved lung repair ability and recovered faster than mice that did not receive the drug.
“This opens up an entirely new direction for potential treatment of IPF,” said lead author Santu Yadav, PhD, assistant professor of medicine at the Tulane University School of Medicine. “Instead of using drugs to kill senescent cells, we are re-activating our own immune system to clear them out.”
More research is needed to determine the efficacy of drugs that target CTLA4 or other so-called “checkpoint proteins” to rejuvenate the immune system. A primary concern is determining a safe dosing strategy that allows for the immune system to attack senescent cells without causing harmful levels of inflammation.
IPF is a disease of aging and is rarely seen before age 50. These findings also offer hope that this approach could work for other similar aging related diseases.
“If it works in IPF, this immune rejuvenating approach to treatment may be effective in other diseases such as Alzheimer’s or cardiovascular diseases in which senescent cells are known to accumulate,” Thannickal said. “Can the right drug activate T cells in a way that clears senescent cells without causing collateral damage? If so, we may be closer to combating many aging related diseases and perhaps even aging itself.”
Source: Tulane University


