
By Biénne Huisman for Spotlight
Scientists worldwide are sounding the alarm at the return of syphilis, describing the comeback of the easily preventable infection as a huge public health failing – as an effective vaccine remains elusive.
Syphilis, one of the oldest known diseases, is making a resurgence worldwide. Top global scientists described this as a public health crisis and failure, given that the sexually transmitted infection (STI) – which can have dire and fatal consequences especially for newborn babies – is curable with early treatment.
The return of syphilis was under discussion at the 2024 Conference on Retroviruses and Opportunistic Infections (CROI) where scientists, clinicians, and public health advocates gathered in Denver in March.
Addressing delegates in the Colorado Convention Centre, Professor Khalil Ghanem of Johns Hopkins University School of Medicine in Baltimore, noted a paucity of data – while syphilis continues to increase with “clinicians caring for patients with complex clinical presentations”. Ghanem was pointing out that there is little systematic information on how to manage cases of advanced syphilis, like neurosyphilis (syphilis in the central nervous system) and ocular syphilis (syphilis in the eyes).
Among some medical practitioners, syphilis is known as “the great imitator” due to its variable clinical manifestations that can mimic other diseases. In its severe forms, it can cause chronic multiple organ damage in adults. The infection can also be passed on from a mother to her baby during pregnancy resulting in congenital syphilis, causing premature birth, miscarriage, stillbirth, and birth defects. In most cases, however, the bacterial infection is transmitted sexually. Transmission can be prevented through the correct use of condoms.
According to the World Health Organization (WHO’s) latest available figures for congenital syphilis – dated 2016 – globally there were an estimated 661 000 congenital syphilis cases that year; including 143 000 stillbirths, 61 000 neonatal deaths (a newborn baby dying within seven days) and 109 000 surviving infants with a clinical diagnosis. Spotlight recently reported on a rise in sexually transmitted infections in Gauteng and in 2021 published an in-depth article on congenital syphilis in South Africa.
‘A failure of the healthcare system’
Epidemiologist Alex de Voux, from the University of Cape Town, moderated a session on syphilis at CROI. Speaking to Spotlight between sessions, an impassioned De Voux said the return of syphilis is “a failure of healthcare systems (in South Africa and abroad) – because we have the tools, we know how to test for it, and we know how to treat it”.
She added: “The most extreme outcomes of congenital syphilis are stillbirths and neonatal deaths. We don’t even really understand the extent of longer term outcomes: neurological complications, skeletal deformations, impaired mental health development… And all these significant complications arise from an easily preventable infection. Remember, we use penicillin, which has been around for ages. The treatment hasn’t changed in all this time.”
Figures presented at CROI include from the Centers for Disease Control and Prevention in the United States, reporting a 76% increase in syphilis cases between 2013 and 2017. The WHO estimates that 7.1 million people between 15 and 49 years old were infected with syphilis in 2020. (See a WHO fact sheet on syphilis here.)
In 2018, at least 33 927 cases of syphilis were reported in 29 European Union member states, as recorded by the European Surveillance System (TESSy), at a rate of seven cases per 100 000 population. The reported syphilis rates were nine times higher in men than in women; showing a peak onset age of 25 to 45 years, in men.
Syphilis and HIV
One study presented at the conference surveyed 20 000 MSM (men who have sex with men) across ten cities in India, noting dramatic increases in syphilis in every city. It found syphilis was most prevalent in older MSM, pointing to a need for STI control efforts in this population. “Among people living with HIV, syphilis infection was associated with elevated (HIV) viral loads, raising concerns for transmission of HIV,” the study authors wrote.
Another study conducted in Cologne in Germany investigated 60 patients co-infected with syphilis and acute HIV. The study cites “rising co-infection rates and the unique interaction between these two sexually transmitted infections. Syphilis enhances HIV transmission and acquisition, while HIV accelerates the progression of syphilis…”
An ancient condition, the oldest artistic representation of syphilis is considered to be on a Peruvian jug dating back to the 16th century, depicting a mother suffering from syphilis holding a child. Famous people who had syphilis include Oscar Wild and Friedrich Nietzsche. [Read about the history of syphilis here]. Infections dropped sharply with the availability of penicillin in the 1940s.
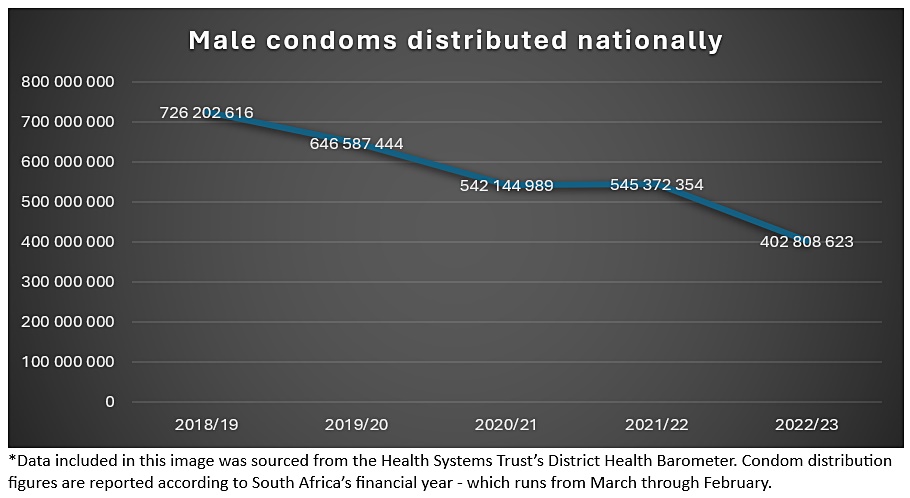
However, over the past two decades scientists have reported an alarming spike in cases. This has been attributed by some to a drop in condom use. The reasons for a decrease in condom use is not clearly understood – one possible factor is a false sense of security given lower HIV transmission rates, effective HIV treatment, and the availability of HIV transmission prevention in the form of pre-exposure prophylaxis (PrEP). PrEP contains a combination of two antiretroviral medicines which are highly effective at preventing HIV infection when taken as prescribed by someone not living with HIV, while not offering protection against other STIs like syphilis. Access to condoms may also be a factor. As Spotlight recently reported, the number of condoms distributed by the South African government has decreased dramatically over the last five years.
Sex partners
One study presented at CROI found: “The risk factors associated with acquired syphilis are sexual behaviour, serosorting (a strategy that involves selecting sexual partners of the same HIV status) among people living with HIV, multiple sexual partners, the use of PrEP to compensate for HIV risk behaviour, and social networking sites or mobile device apps to find sex partners.”
At the syphilis session at CROI, Dr Angélica Espinosa Miranda, STI unit coordinator at the Brazilian Ministry of Health, presented a talk titled “The Burgeoning Epidemic of Congenital Syphilis”. She emphasised “the underdiagnosis of syphilis in pregnancy, especially in regions with limited healthcare access”.
Miranda’s statement resonates with De Voux’s research in South Africa, which found congenital syphilis cases to be gravely underreported in the country. Congenital syphilis is a notifiable condition in South Africa, meaning that if a doctor delivers a baby believed to be infected they are required by law to report it to the National Institute For Communicable Diseases. De Voux’s study relays how reported congenital syphilis cases in South Africa’s healthcare system between January 2020 and June 2022 – 36 cases for every 100 000 live births – were at least half the figure estimated by WHO scientists – thus bolstering the hypothesis that there is a high number of undiagnosed syphilis in South Africa.
Penicillin treatment
In her talk, Miranda added that ensuring that infected pregnant women receive timely and appropriate penicillin treatment is critical to preventing congenital syphilis. “Penicillin is the only effective treatment during pregnancy,” she said. “However challenges remain, such as limited healthcare access and penicillin shortages in some countries.”
When penicillin cannot be used (due to unavailability in a country or allergy in a patient) the WHO’s STI guidelines suggest using doxycycline 100mg twice daily orally for 30 days.
Penicillin shortages are a problem worldwide, and in South Africa too. “South Africa has also been affected by shortages of penicillin,” says De Voux. “In fact, often they will make sure that they keep stocks and prioritise pregnant women. So that means that sometimes other people who are infected with syphilis will get treated with something that’s much more burdensome. Instead of having penicillin injections, they will take oral tablets – doxycycline – which has these gastrointestinal side effects, so an upset stomach. You have to try minimise the side effects with f ood.”
Miranda stressed the need to invest in developing new strategies – antibiotics apart from penicillin – to treat syphilis. Meanwhile, epidemiologists agree that a vaccine for syphilis is important but that this scientific solution remains elusive.
Republished from Spotlight under a Creative Commons licence.
Source: Spotlight

